As a practicing obstetrician-gynecologist for over 30 years, I’ve seen uncountable cases of endometriosis, and I know how life-altering a diagnosis can be. At its worst, endometriosis is debilitating, severely painful, and can affect every facet of a patient’s life: their careers, their home life and hobbies, their relationships and sex life, their education, their potential to become parents.
Unfortunately, many patients spend years living with extremely painful periods, infertility, excessive menstrual bleeding, fatigue and other symptoms of endometriosis, silently suffering under the impression that they simply “get bad periods.” Other patients may be mistakenly told there’s no recourse beyond over-the-counter pain medication, or may even have resigned themselves to living with a “mystery” condition.
But “living with” endometriosis symptoms doesn’t have to be a life sentence. There is hope, and there are options. I believe that, in the vast majority of cases, an endometriosis patient’s quality of life can be significantly improved with treatment. While we still don’t know exactly why endometriosis occurs, we do have a variety of non-surgical and surgical means to manage the pain and discomfort associated with this troubling condition. With a compassionate approach and a meticulous investigation into a patient’s case, I am certain that endometriosis symptoms can be managed and improved, providing the patient with much-needed — and much-deserved — relief.
To help you better understand endometriosis, its symptoms and your treatment options, I’ve answered some of the most common questions about the condition below. If you have questions specific to your situation or symptoms, please don’t hesitate to reach out to schedule an appointment with me or another experienced physician at Denali.
- What is endometriosis?
- What are the symptoms of endometriosis?
Who is most at risk for endometriosis? How is endometriosis diagnosed? How is endometriosis treated?
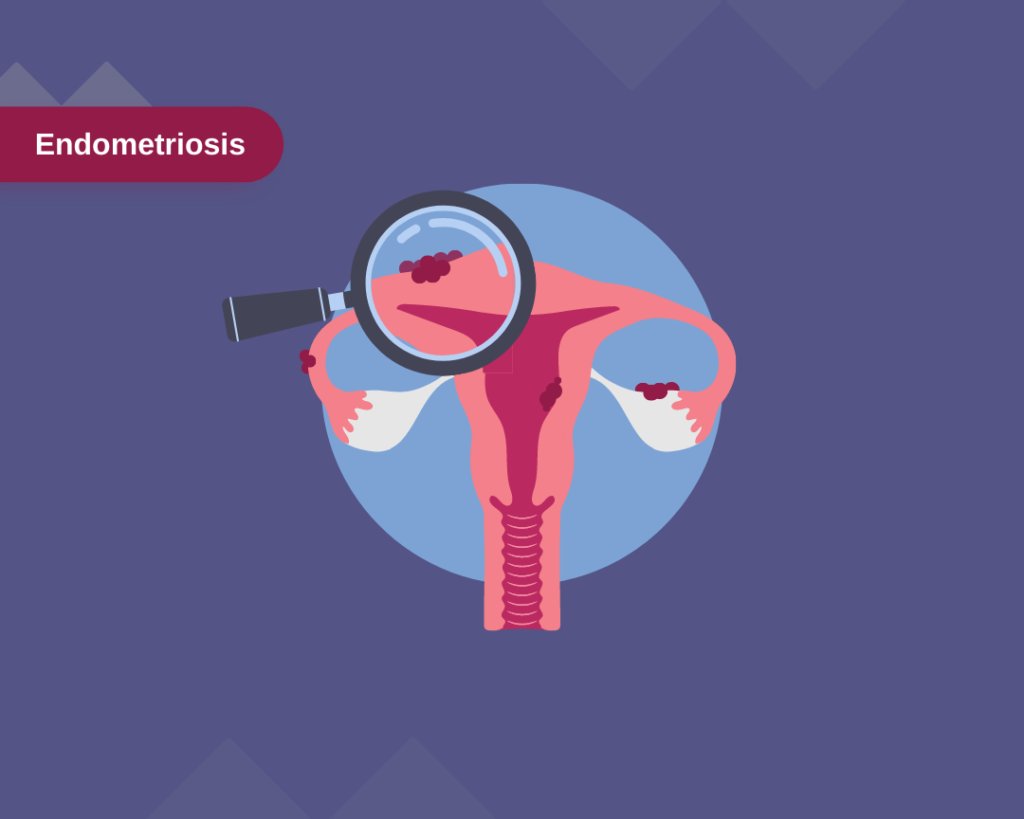
What is endometriosis?
Endometriosis is a condition that affects up to 10% (190 million) of American women. Endometriosis occurs when tissue that normally grows inside the uterus, or endometrium, grows irregularly outside the uterus. Endometriosis usually involves the ovaries, fallopian tubes and the tissues lining the pelvis. Much more rarely, endometrial-like tissue may be found beyond the area where pelvic organs are located, like the cervix, rectum, bladder, intestines, stomach, vagina, and vulva.
When endometriosis occurs, the endometrial-like tissue behaves as it would inside the uterus—meaning it thickens, breaks down, and bleeds with each menstrual cycle. Unlike normal endometrial tissue, though, this tissue has no way to exit the body. When this trapped abnormal tissue builds up outside the uterus, it can lead to inflammation, scarring, and painful cysts. The irritated tissue around these growths may develop adhesions, which are bands of fibrous tissue that can cause pelvic tissues and organs to “stick” to each other. Unfortunately, this sounds uncomfortable because it is. Endometriosis is often painful — sometimes severely so — particularly during menstrual periods when bleeding and shedding of endometrial tissue is triggered.
What are the symptoms of endometriosis?
The primary symptom of endometriosis is pelvic pain, usually associated with menstrual periods. Patients suffering from endometriosis will often report cramping during their period that is much worse than what they’d consider “normal” for their cycle. As new abnormal tissue grows and scar tissues and/or cysts develop, a patient’s pain may increase.
Diagnosing endometriosis can sometimes be tricky, as it is often mistaken for other conditions that cause pelvic pain, like pelvic inflammatory disease (PID) or ovarian cysts. It may also be confused with irritable bowel syndrome (IBS), the symptoms of which include diarrhea, constipation and abdominal cramping. IBS can also accompany endometriosis, which can further complicate the diagnosis.
In general, the common signs and symptoms of endometriosis include:
- Painful periods (dysmenorrhea). Pelvic pain and cramping may begin before and continue several days into a menstrual period. This may also present as lower back and abdominal pain.
- Pain with intercourse. Pain during or after sex is common with endometriosis.
- Pain with bowel movements or urination. Typically, more common during menstrual periods.
- Excessive bleeding. Especially heavy menstrual periods or bleeding between periods (intermenstrual bleeding) may occur with endometriosis.
- Infertility. Endometriosis is one of the most common conditions linked to female infertility, affecting a massive 24% to 50% of women with infertility. Mild to moderate cases may only cause temporary infertility that can be corrected with treatment. Surgery to remove the endometrial tissue can help increase the chances of pregnancy.
- Other signs and symptoms include fatigue, diarrhea, constipation, bloating or nausea, especially during menstrual periods.
I would like to note here that, although pain is an extremely common symptom of endometriosis, the severity of your pain does not necessarily correlate with the severity of your condition. One patient could have a mild case of endometriosis but experience severe pain; likewise another patient could have advanced endometriosis with little or no pain. It is important to know that your experience with endometriosis symptoms is valid regardless of how much pain you are currently experiencing. Every case of endometriosis is unique, and every case deserves to be treated with compassion, kindness and a dedication to finding treatment that improves your quality of life.

Who is most at risk for endometriosis?
Anyone of reproductive age who has a uterus could potentially develop endometriosis, but there are some factors that can put a person at a higher risk of developing the condition, including:
- Starting menstruation at an early age (before age 11)
- Starting menopause at an older age
- Never giving birth
- Having one or more close female relatives (mother, sister or daughter) who have endometriosis
- Having an abnormal uterus as diagnosed by a doctor
- Shorter menstrual periods (less than 27 days)
- Heavier menstrual periods lasting more than 7 days
- Having higher levels of estrogen, or a greater lifetime exposure to estrogen produced by your body
- Low body mass index
- Having any medical condition that prevents the passage of blood from the body during menstrual periods
- Having one or more disorders of the reproductive tract
Endometriosis usually develops several years after the first menstrual period. Symptoms may temporarily improve with pregnancy and breastfeeding (though they can return after breastfeeding has concluded,) and may go away completely with menopause unless the patient is taking estrogen.
How is endometriosis diagnosed?
If your doctor suspects you may have endometriosis based on your history, symptoms and physical exam. A laparoscopy is used and, typically, a biopsy to diagnose the condition. A laparoscopy is a minimally invasive procedure involving a small incision made under general anesthesia. The incision is made near the navel so a very small, thin camera can be inserted in and around the uterus. If your doctor does find signs of abnormal tissue growth, they will excise the endometriosis and send it for pathological study.
Because a biopsy is a diagnostic requirement of endometriosis, there are no non-surgical means of obtaining a positive diagnosis. However, physicians do use other non-surgical diagnostic imaging to check for signs of endometriosis, including:
- Pelvic exam. During a pelvic exam, the physician manually feels areas in the pelvis for abnormalities, like cysts on the reproductive organs or scars behind the uterus.
- Ultrasound. To obtain ultrasound imaging, a small wand called a transducer is either externally pressed against the abdomen or inserted into the vagina to visualize the uterus, pelvic area and reproductive organs using high-frequency sound waves. An ultrasound won’t definitively tell your physician that you have endometriosis, but it can identify cysts associated with endometriosis.
- Magnetic resonance imaging (MRI). This noninvasive scan of the internal organs and tissues uses magnetic waves and radio waves to create detailed imaging. MRI can be helpful prior to surgical treatment of endometriosis, as it can provide your surgeon with detailed information about the size and placement of abnormal tissue.

How is endometriosis treated?
As a physician and as a woman, I know how daunting an endometriosis diagnosis can be. Fortunately, effective treatments are available to help patients manage their condition and minimize pain, to give you as much relief as possible from your symptoms.
When I work with endometriosis patients, I like to think of myself as walking alongside them, using my years of experience and advanced training to bring them the best possible treatment and, hopefully, results. Each course of treatment is highly individual to the patient
in question and is informed by many different factors including the patient’s age, the severity of their symptoms, and whether they hope to become pregnant in the future.
Most doctors, myself included, will start with a more conservative approach to treatment. This usually means starting the patient on pain medications and/or hormone therapy, and opting for surgery only if the initial treatment fails to provide relief.
Non-Surgical Treatment Options
- Pain medication. Over-the-counter pain relievers like ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve) may be recommended or prescribed to help ease painful menstrual cramps.
- Hormone therapy. Hormone therapy may be recommended in combination with pain medication if the patient is not trying to get pregnant. This may include:
- Hormonal contraceptives like birth control pills, patches or vaginal rings.
- Gonadotropin-releasing hormone (Gn-RH) agonists and antagonists, which shrinks endometrial tissue by blocking the production of ovarian-stimulating hormones, lowering estrogen levels and preventing menstruation. Because these drugs create an artificial menopause, many patients also take a low dose of estrogen or progestin along with Gn-RH agonists and antagonists to decrease side effects like hot flashes, vaginal dryness and bone loss.
- Progestin therapies, which are available in many delivery methods including an intrauterine device with levonorgestrel (Mirena, Skyla), contraceptive implants (Nexplanon), contraceptive injections (Depo-Provera) or progestin pills (Camila). These therapies can stop periods and endometrial implant growth, which can help relieve symptoms.
- Aromatase inhibitors, medicines that reduce the amount of estrogen in the body. Your doctor may recommend an aromatase inhibitor in addition to a progestin or combination hormonal contraceptive.
Because there is no definitive cure for endometriosis at this time, I prioritize communicating with my patients about the pros and cons of each type of treatment for their specific symptoms and needs. I make sure to talk through their current and future lifestyle and family plans to get a better sense of which treatments will be most suitable. It’s important that patients know their symptoms can return. If treatment is stopped, for example, if a patient wants to try to get pregnant, they would need to stop their hormone therapy treatment, during which time their symptoms may recur.
If non-surgical treatment fails, or if a patient is suffering from severely painful symptoms, it may be time to consider a surgical approach.
Surgical Treatment Options
Surgery is almost never the first line of defense against endometriosis, particularly because symptoms can and often do recur even after surgery. If we’re looking at a surgical option, conservative surgery is the place we start. “Conservative surgery” describes the surgical removal of abnormal endometrial tissue growths while preserving the uterus and ovaries. Conservative surgery may increase the chance of conception in patients who are trying to become pregnant.
A laparoscopic surgery is the most common surgical method of treating endometriosis because it is minimally invasive. During this procedure, a surgeon makes a few small incisions in the abdomen. The surgeon will insert a thin tube with a light and a camera into one incision. Small tools are then inserted in the incision to aid the removal of endometrial tissue (excision). The surgeon can also remove any scar tissue that has built up in the area for additional symptom relief.
I prefer laparoscopic surgeries for their shorter recovery time and smaller scars compared to traditional open surgery (laparotomy), which involves a larger incision and therefore a larger scar and longer recovery. In some very extensive cases of endometriosis, a surgeon may need to perform a laparotomy instead of a laparoscopy, but this is exceedingly rare. Even in very severe cases of endometriosis, most can be treated laparoscopically by a minimally invasive trained surgeon.
Finally, a hysterectomy is considered a last-resort option for treating extremely severe cases of endometriosis. Surgery to remove the uterus (hysterectomy) with removal of the ovaries (oophorectomy) is only considered as a treatment option when a patient is experiencing debilitatingly severe pain and/or extensive scarring and cyst development, i.e. patients that have not experienced meaningful relief through other, less invasive treatments.
While it’s true that a hysterectomy will stop the release of hormones and trigger menopause, improving endometriosis pain for some patients, it is by no means a “quick fix” or “easy solution.” For some patients, abnormal tissue that remains after surgery may continue to cause symptoms. Early menopause carries significant risks — especially in those who undergo a hysterectomy before the age of 35 — including heart and blood vessel (cardiovascular) diseases and certain metabolic conditions. Surgical menopause can be treated with hormone replacement to decrease many of these risks.
I think of hysterectomy as the “nuclear option” in endometriosis treatment, which is why I don’t recommend it to any patients whose symptoms may be treated equally as effectively through non-surgical or minimally invasive methods. While we may eventually determine that major surgery is warranted, I think most patients would agree that they’d prefer treatment options that don’t leave them down an organ at the end of the day! A hysterectomy is a major surgery and a life-altering change physically, emotionally and to your family planning. It is a serious decision; so I prefer to educate my patients then work together to try other means of managing their symptoms and achieve a better, more pain-free quality of life. There is absolutely hope for endometriosis without necessitating serious surgery, and I am passionate about helping my patients find relief through whatever means are best for them.

Final Thoughts
Endometriosis can be scary, especially when you are navigating painful symptoms without guidance. But you don’t have to suffer through this alone, or without help! I wrote this blog specifically because it is important to me that patients experiencing these symptoms can easily find the resources they need to get treatment and relief. I hope to help ease the fears of my patients and provide a light in the dark through compassionate, patient-focused treatment.
My goal is to listen to you with empathy and use my lifetime of experience to build a treatment plan specifically tailored to you. If you’re experiencing
endometriosis-like symptoms, I would be honored to help start you on the path to a less painful quality of life. Contact the team at Denali OB-GYN to schedule an appointment with me or with any of our knowledgeable physicians. There is hope for endometriosis, and it starts here!